Outstanding long-term results verified by published research
63%
REDUCTION IN DEPRESSION
Mindfulness Journal 2018 | RCT Study | School of Psychology | University of Surrey
40%
REDUCTION IN STRESS
BMJ Open 2013 | Evaluation Study | Department of Psychiatry | University of Oxford
26%
REDUCTION IN FATIGUE
Journal of Occupational Health Psychology 2016 | RCT Study | School of Psychology | University of Surrey

An approach that works
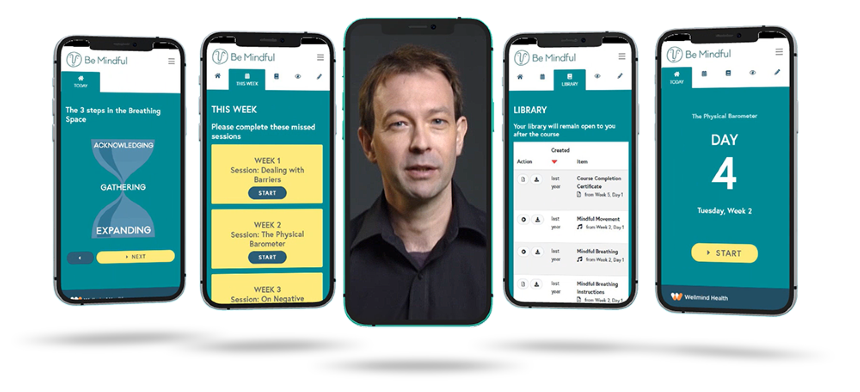
Participants engage with videos and interactive sessions where they practice an effective way of handling stress and the challenges of life.

Completed at own pace
Web-based and on-demand, the 4-week Be Mindful program can be followed at a pace that suits individuals, using any desktop or mobile device.

Monitor progress and results
Participants measure their progress and outcomes during and after the program which are reported to their healthcare sponsor.